Anorectal Conditions Treatment in Vizag
Introduction
Anorectal conditions refer to disorders that affect the anus and rectum, often causing discomfort, pain, or bleeding. These issues are more common than many realize and can significantly impact a person’s daily life and well-being. While some anorectal conditions are mild and resolve with lifestyle changes or medication, others may require medical or surgical intervention. Early diagnosis and treatment are essential to prevent complications and improve quality of life.
Common Anorectal Conditions:
Several anorectal disorders are frequently encountered in clinical practice, including:
- Hemorrhoids or Piles
- Swollen veins in the rectum or anus that may bleed, pain or cause discomfort.
- They are a common condition affecting millions of people, often due to straining during bowel movements, chronic constipation, pregnancy, or prolonged sitting.
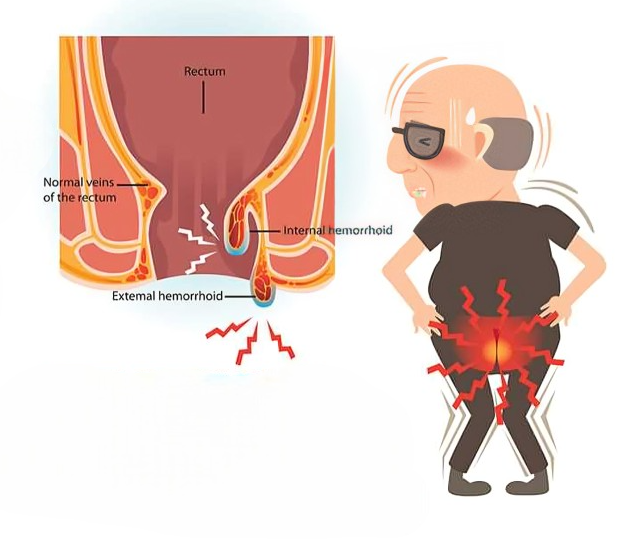
- There are two main types of hemorrhoids:
- Internal hemorrhoids, which occur inside the rectum and may not be immediately visible or painful but can cause bleeding.
- External hemorrhoids, which form under the skin around the anus and can be painful, itchy, or even develop clots (thrombosed hemorrhoids).
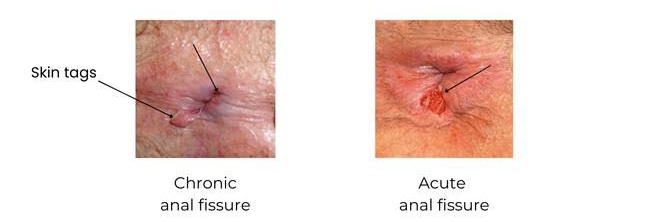
Anal Fissure
- A small tear in the lining of the anus causing pain during bowel movements (passing stool/motion).
- Patient’s typical symptoms are severe pain after passing motion, burning sensation, itching and occasionally blood drops with stool.
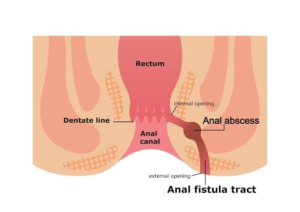
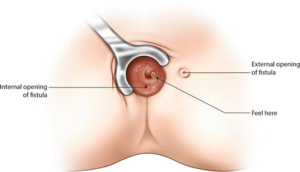
Fistula
- An abnormal connection between the anus and surrounding tissues. This condition often results from an infection that did not heal properly, leading to the formation of an abscess and a persistent drainage channel which is tubulised into a permanent tract and requires surgical intervention.
- Symptoms may include: pain/ swelling around anus, recurrent abscess (cavity with pus), discharge of pus/ blood, irritation.
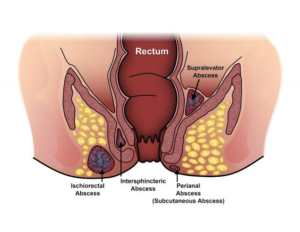
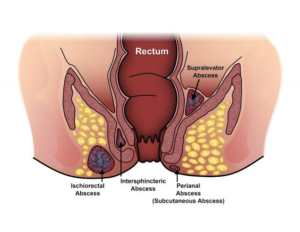
Perianal / Ischiorectal Abscess
- A perianal abscess is a painful collection of pus near the anus, caused by an infection in the small anal glands. When the infection spreads deeper into the surrounding tissues, it may become an ischiorectal abscess, located between the rectal muscles and deeper tissues of the buttocks.
- Both conditions are forms of anorectal abscesses, and they typically require prompt medical treatment to prevent complications.
Causes
- These abscesses are usually caused by:
- Blocked anal glands
- Bacterial infections (common gut bacteria)
- Inflammatory bowel diseases (e.g., Crohn’s disease)
- Trauma or anal fissures
- Immunocompromised states (like diabetes or HIV)
Symptoms
- Common signs and symptoms include:
- Severe pain around the anus
- Swelling and redness near the anal area
- Fever and chills
- Painful bowel movements
- A visible lump or boil near the anus (especially in perianal abscess)
- If left untreated, the abscess may rupture or lead to a chronic fistula
Need Help?
We’re Just a Call Away!
When is Surgery Needed?
Surgical intervention is considered when conservative treatments fail to relieve symptoms or when complications arise. Persistent pain, recurrent bleeding, or chronic infections that do not improve with medication or lifestyle modifications often indicate the need for surgery. Hemorrhoids that are large or unresponsive to conservative treatment may require surgical removal. Anal fissures that do not heal with topical treatments, and most anal fistulas, especially those associated with recurring abscesses, often need surgical intervention to prevent ongoing infection and complications. Perianal and ischiorectal abscesses typically require prompt drainage to relieve pain and prevent the spread of infection. Timely surgical care reduces the risk of chronic symptoms and further health issues.
Treatment Options
1. Non-Surgical Treatment
These are effective for mild to moderate hemorrhoids and anal fissure. It is also followed in post-operative perianal cases.
- Lifestyle & Dietary Changes: Increasing fiber intake, staying hydrated, and avoiding straining for passing stool/ motion.
- Topical Medications: Creams/ ointments to relieve pain and inflammation.
- Sitz Baths: Warm water baths to soothe the affected area and relieving spasm of muscles.

2. Surgical Treatment
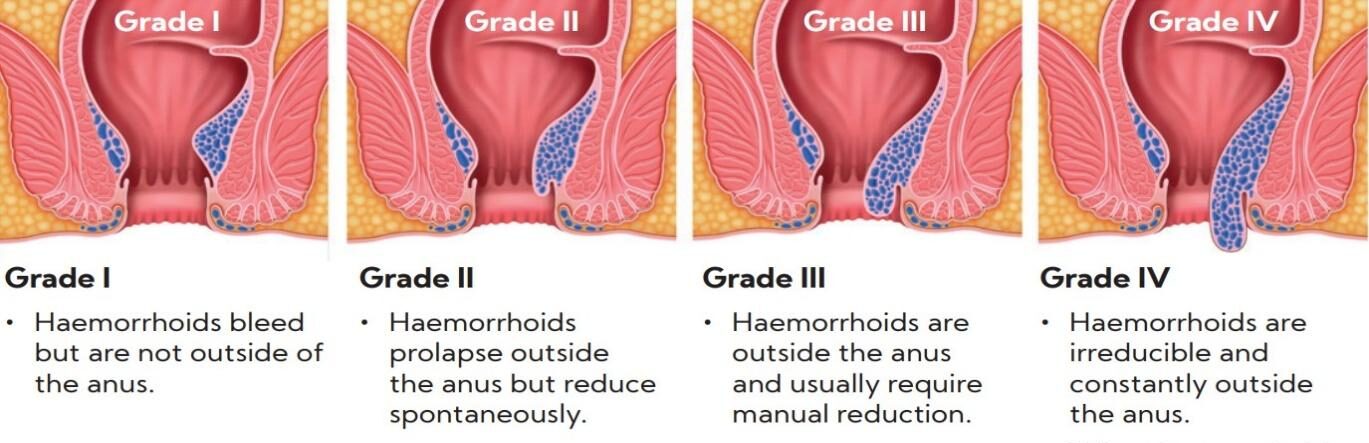
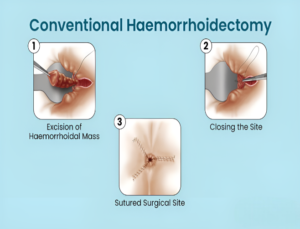
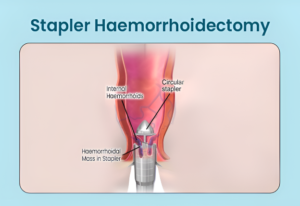
Hemorrhoids : Recommended for severe, persistent, or recurring hemorrhoids:
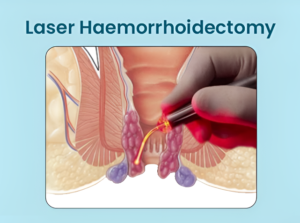
- Laser Hemorrhoidoplasty: A minimally invasive procedure using laser energy to shrink hemorrhoids with minimal pain and faster recovery.
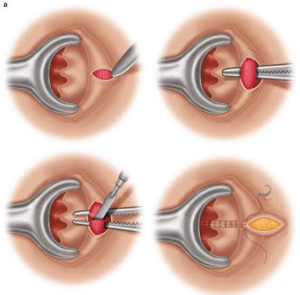
- Hemorrhoidectomy: Surgical removal of large or painful hemorrhoids. This is effective for grade 3 or 4 hemorrhoids and those not responding to other treatments.
- Stapled Hemorrhoidopexy: A procedure that repositions and staples the hemorrhoidal tissue, reducing blood flow and shrinking it over time.
- Sclerotherapy: A sclerosant is injected directly into the hemorrhoidal tissue which causes the blood vessels to shrink, collapse eventually.
1. Anal Fissure:
Chronic fissures or those resistant to medical treatments may require:
Lateral Sphincterotomy : A small portion of the anal muscle is carefully cut to relieve spasm and promote healing. It is the most effective long-term solution with high success rates.
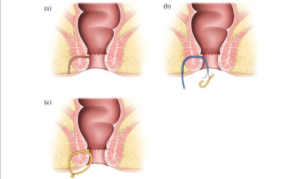
2. Anal Fistula
Treatment depends on the type and severity of the disease.
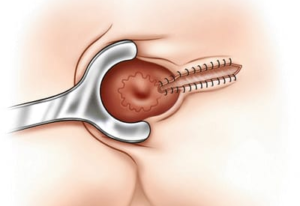
- Fistulotomy/ Fistulectomy : The most common procedure. The fistula tract is opened or removed in-toto and allow it to heal naturally. Ideal for simple fistulas.
- Laser Fistula Treatment : A minimally invasive option using laser energy to seal/ burn the tract from the inside. It offers faster recovery and minimal pain.
- Seton Placement : Used for complex or deep fistulas. A soft thread is placed in the tract to keep it open and help it heal over time.
3. Perianal/ Ischeorectal Abscess
- Incision & Drainage : The primary treatment of abscess anywhere in body is drainage procedure, where a small cut is made to drain the pus. It provides immediate relief and helps prevent the spread of infection. Sometimes, wound is quite big due to delayed presentation. To prevent soakage of the wound with stool (motion) and prevent aggravation of sepsis, diversion of intestine is needed – colostomy (large intestine is opened outside abdomen and motion is allowed to collect in the bag). Once the wound improves or heals fully, colostomy is reversed – to attain continuity of the intestine.
- Antibiotics : Antibiotics alone are usually not enough without drainage. Used in combination with drainage or when signs of a broader infection (like fever) are present.
- Fistula Evaluation : After the abscess heals, a follow-up may be needed to check for an anal fistula, which can develop in some cases and may require further treatment.

Recovery & Aftercare
Recovery depends on the treatment type. Most non-surgical treatments allow a quick return to daily activities. Surgical procedures may require a few days to a week of rest.
Conclusion
Don’t neglect persistent perianal pain/ bleeding or discharge from anal region. Timely diagnosis and treatment of anorectal conditions are essential to avoid complications and improve comfort.
Our team provides personalized care instructions and follow-up support to ensure complete recovery and long-term relief. We prioritize your comfort, privacy, and long-term well-being.
Book your consultation today and get lasting relief from anorectal issues at “Vizag Surgicare”.
contact us
Get In Touch With Us
phone number
Mobile No 1 : +91-9849239213
Mobile No 2 : +91-9848638615
our address
First Floor, Mohan Medical Shop, Seethammadhara (NE), Visakhapatnam-530013
email address
info@vizagsurgicare.com
